Atlanta VBAC Protocol
Preparing for a VBAC: An Evidence-Based Checklist
This guide is educational and not medical advice. Always review choices with your clinician.
VBAC isn’t just possible, it’s powerful! We know this because between the two of us, we’ve supported dozens of VBAC families here in Atlanta, and Milene is a VBAC mom herself. The families who come to us are determined: they want solid information, supportive providers, and a team that believes in them. And they deserve it. You deserve it.
Many families first find us as Atlanta doula photographers, because we’ve learned how to weave together hands-on support and storytelling. We’re asked about VBAC often, and it has become one of the areas where we serve most.
Because VBAC comes up so often in our work, we wrote this guide. It’s a quick reference to guide parents to for the answers, resources, and encouragement families keep looking for. Too often, outdated myths or hospital policies make VBAC sound out of reach. The evidence tells a different story. This guide can give you the clarity, tools, and confidence you need to prepare well.
Cuddles = oxytocin = powerful labor hormone
Quick VBAC facts
VBAC is safe and possible for many families. Success rates are often quoted around 60–80%, depending on your personal history and circumstances (ACOG).
Uterine rupture is rare — about 0.4–0.9% in spontaneous VBAC labors with a low-transverse scar. The risk does increase with some induction methods (NIH).
Epidurals are allowed in VBAC labors and don’t hide the usual warning signs of rupture (most often picked up on the fetal monitor) (RCOG).
Induction is possible after cesarean, but not all methods are safe. Misoprostol (Cytotec) should not be used at term; mechanical methods like a Foley balloon and cautious oxytocin may be offered (ACOG).
Joy finding out she is 10cm!
Quick VBAC checklist
Find a VBAC-supportive provider & hospital
Gather your cesarean records
Add a doula & support group
Daily movement + positioning
Chiro, PFPT, and massage
Prep your mind with facts, therapy, affirmations & meditation
Talk through TOLAC, induction and monitoring ahead of time
Excited that her birth day is finally here.
Find your VBAC-supportive team
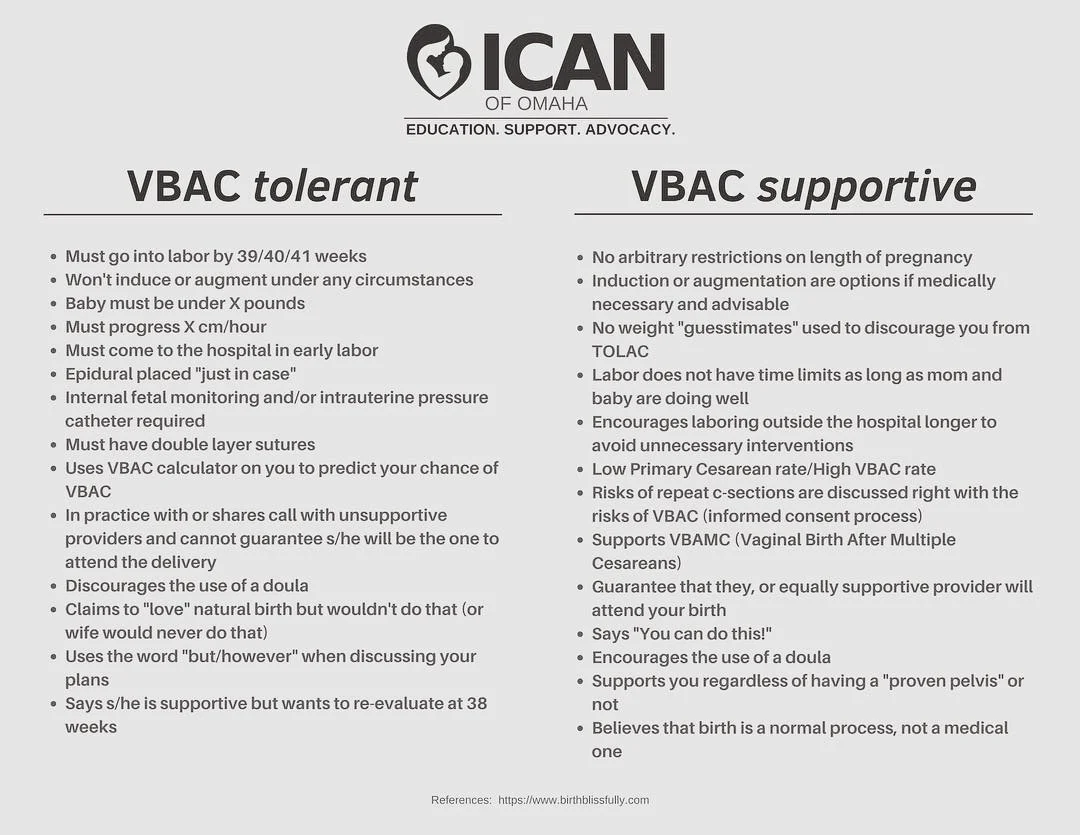
Not all providers approach VBAC the same way. Some actively support it, others tolerate it quietly, and some simply don’t offer it.
Questions to ask:
What’s your VBAC success rate?
What’s your approach to induction?
How do you handle emergencies or “off-script” labors?
Professional guidance is clear: ACOG (in the U.S.) and RCOG (in the UK) both say VBAC is a reasonable and supported option when resources are in place.
Find Other VBAC families:
ICAN (International Cesarean Awareness Network) offers education, advocacy, and a network of families who’ve been there.
ICAN of Atlanta is our local chapter, with meetings and a supportive community.
Staying nourished and using the toilet to help dilation.
Home or Hospital Birth for VBAC?
One of the most frequent questions families ask is: “Should I plan a home birth or hospital birth for my VBAC?” There’s no one-size-fits-all answer, it depends on your health history, comfort level, and the team you trust.
Hospital VBAC: Many choose hospital settings because the backup of immediate medical resources is available. The trick is finding a hospital and provider who genuinely support VBAC—because policies and attitudes vary widely.
Home VBAC (HBAC): Some families opt to birth at home with a skilled midwife, valuing the freedom and fewer interventions. But safety depends heavily on screening, transfer plans, and clear communication with providers.
We’ve written a deep dive on HBAC (Home Birth After Cesarean) that explores FAQs, statistics, and what to discuss with your midwife. You can read it here: HBAC FAQ + Stats.
In that article, you’ll find stories, success data, and real client questions—perfect to compare with your VBAC path.
Roaring her baby out
Key questions to ask
How many VBACs have you attended recently?
What’s your VBAC success rate?
How do you handle inductions in VBAC labors?
What happens here if I need an urgent cesarean?
How do you use VBAC calculators; as a conversation tool, or as a cutoff? (They should be a tool only, not a gatekeeper.)
Realization that she got her VBAC!
Gather your records
Get a copy of your cesarean operative report. It will note incision type (low-transverse vs. classical), adhesions, and other details that matter for planning.
Check your birth spacing. If your last birth was not that long ago, that’s a talking point for your care team. It doesn’t rule out VBAC, but it changes what some practitioners may suggest.
Bodywork & alignment
We highly recommend you add bodywork as part of VBAC prep. It doesn’t guarantee anything, but it helps many people feel more balanced and comfortable heading into labor.
Webster-certified chiropractic: Find a provider here.
Pelvic floor PT: helps with strength, mobility, and scar tissue.
Myofascial or abdominal massage: reduces tension and adhesions.
Spinning Babies® positions: Flip a Breech resource.
Literal Bliss
Prepare your mind and emotions
VBAC isn’t just physical, it’s emotional. You may carry fears from your last birth or worry about how this one will unfold. That’s normal.
Hypnobirthing, affirmations, visualization: tools to calm your nervous system. Try the Hypnobabies Breech Baby track for focused support.
Support groups: ICAN and ICAN of Atlanta are incredible for hearing real VBAC stories.
Doula support: Continuous support during labor lowers cesarean rates and improves outcomes (Cochrane Review).
Daily movement & lifestyle
Steady, simple habits matter more than fancy protocols.
Walk daily. Stretch. Move in ways that feel good.
Use positions that open the pelvis (lunges, hands-and-knees, side-lying).
Practice breath work: connecting diaphragm and pelvic floor.
Fuel your body with protein, iron, hydration, and real rest.
Make a plan with your provider
It helps to talk through these ahead of time so you’re not surprised in the moment:
Induction & augmentation: Which methods do they offer? (No misoprostol; maybe Foley balloon or oxytocin.)
Monitoring: Continuous fetal monitoring is standard in VBAC labors (RCOG).
Pain relief: Epidurals are safe for VBAC and don’t block rupture signs (ACOG).
Gestational age: VBAC rates dip after 40 weeks, but dates alone shouldn’t rule you out (RCOG).
Twins or unknown scar type: Sometimes still possible, depends on details (ACOG).
Why many families choose VBAC
To avoid another surgery and the longer recovery that can follow.
To lower the risks in future pregnancies, especially placenta issues tied to repeat cesareans (NIH).
To experience vaginal birth itself, which can be healing, empowering, and deeply meaningful.
That said, it’s important to be real: if a TOLAC doesn’t end in VBAC, recovery can be harder than with a planned repeat cesarean (ACOG).
Atlanta & national resources
ICAN (national) - education, support, advocacy.
ICAN of Atlanta - local community, provider reviews
Successful VBAC pose
Final thought
VBAC isn’t just about avoiding another surgery, it’s about writing the next chapter of your birth story with people who truly listen. We’ve walked with many VBAC families here in Atlanta, and what we see again and again is this: when women are supported, respected, and surrounded by steady care, the whole experience changes.
If you’re planning a VBAC in Atlanta, we’d be honored to walk with you as your doulas, and if you wish, as your storytellers through photography.